Who doesn’t love a bright, confident smile? Teeth whitening strips have become a go-to solution for many people looking to enhance their smiles in an easy and affordable way. But before you tear open that box of whitening strips, it’s important to know how to use them properly to avoid mistakes and get the best possible results.
Here’s everything you need to know about whitening strips—from how to apply them to tips for maximizing their effectiveness. By the end of this blog, you’ll feel confident and ready to brighten your smile while keeping your teeth healthy.
What Are Whitening Strips and How Do They Work?
Whitening strips are thin, flexible strips coated with a gel that contains peroxide, the active ingredient that whitens your teeth. Peroxide works by breaking down stains on the enamel, the outer layer of your teeth, to reveal a whiter, brighter surface. These strips are designed to conform to the shape of your teeth, making them effective and relatively easy to use.
The best part? You don’t need a dentist’s appointment or complicated tools to get professional-looking results. Whitening strips are a convenient, over-the-counter option for at-home whitening, perfect for people with busy schedules or tight budgets.
That said, using them incorrectly can lead to uneven whitening or even tooth sensitivity. That’s why understanding the process is crucial!

Step-by-Step Guide on How to Use Whitening Strips
1. Start with Clean, Dry Teeth
Before applying whitening strips, it’s essential that your teeth are clean and dry. Brush and floss your teeth to remove particles that might block the gel from working effectively. Then, gently dry your teeth using a soft cloth or a tissue. Moisture can make the strips less adhesive and reduce their effectiveness, so don’t skip this step.
2. Peel and Align the Strips
Carefully peel the whitening strip off its backing, exposing the gel side. Align the strip with your teeth, making sure it covers all surfaces you want to whiten. Press it down firmly to ensure full contact with your teeth and smooth out any bubbles or folds.
Want the best results? Work carefully to avoid overlapping strips or leaving gaps between teeth.
3. Wait the Recommended Time
Every brand has its own timing recommendations, typically between 30 minutes to an hour. It’s tempting to leave the strips on for longer, but resist the urge! Overusing whitening products can increase sensitivity and won’t necessarily give you brighter teeth.
4. Remove the Strips and Rinse
When the time is up, gently peel off the strips and dispose of them. Rinse your mouth thoroughly to remove any leftover whitening gel. Avoid brushing your teeth immediately after use to minimize irritation, especially if your teeth feel sensitive.
5. Repeat as Directed
Most whitening strip kits suggest daily use for 1 to 2 weeks. Following the full treatment plan is key to achieving and maintaining noticeable results.
Dos and Don’ts of Using Whitening Strips
Now that you know the basic process, here are some additional tips to help you avoid common mistakes and maximize your results.
Do:
- Follow the Instructions: Always read and follow the manufacturer’s guidelines for application time and duration of use.
- Store Strips Properly: Keep them in a cool, dry place to ensure the gel stays effective.
- Maintain Consistency: Use the strips daily for the recommended treatment period to see lasting results.
- Pair with Good Oral Hygiene: Brushing and flossing are essential for maintaining your white smile after treatment.
- Pay Attention to Timing: Choosing to use strips at night can help keep your teeth free from foods or drinks that might re-stain them during the day.
Don’t:
- Brush Too Hard Before Application: Aggressive brushing can wear away enamel and increase sensitivity. Use a gentle hand and a soft-bristled toothbrush.
- Use More Strips Than Recommended: Doubling up or using strips back-to-back won’t speed up the whitening process and can harm your teeth and gums.
- Consume Stains During Treatment: While whitening strips work, steer clear of coffee, tea, red wine, and tobacco, which can counteract their effects.
- Skip Consulting Your Dentist: If you’re unsure whether whitening strips are safe for you, consult your dentist for advice, especially if you have dental work like crowns or fillings.

What to Expect While Using Whitening Strips
Can Whitening Strips Cause Sensitivity?
It’s not uncommon to experience mild tooth sensitivity or gum irritation during whitening treatments. This usually subsides quickly after you finish your treatment. To minimize discomfort, use toothpaste designed for sensitive teeth and follow the instructions carefully.
How Long Does It Take to See Results?
Some people notice a difference after just a few applications, while others need to complete the full course to see results. Factors like the severity of stains and your natural tooth color can affect how quickly you notice a change.
How Long Do Results Last?
The longevity of your whitening results depends on your lifestyle. You can expect whiter teeth for around 6 months to a year, but avoiding staining foods and beverages can help extend your results. Regular touch-ups can also keep your smile bright.
Alternatives and Enhancements to Whitening Strips
While whitening strips are a fantastic option, they’re not the only tool in the whitening toolbox. Depending on your needs, one of the following options might also be worth exploring:
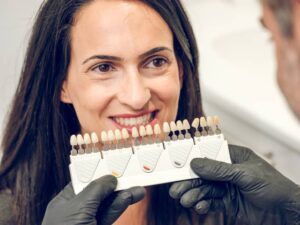
- Professional Whitening Treatments: Available through your dentist for quicker, more dramatic results.
- Whitening Toothpaste: Great for maintenance but unlikely to remove deep stains.
- Custom Whitening Trays: These offer a more personalized fit and are available through your dentist.
- At-Home Laser Kits: A pricier option but can provide quicker results when used with whitening gels.

Final Thoughts
Whitening strips are an accessible and effective way to brighten your smile as long as you use them correctly and follow proper precautions. By keeping your teeth clean, adhering to instructions, and avoiding common mistakes, you can achieve professional-level whitening from the comfort of your home.
Remember, whitening is just one part of oral care. Maintaining overall dental health through regular brushing, flossing, and dental check-ups is crucial for preserving your sparkling smile.
If you have any questions or concerns about whitening strips or maintaining your oral health, don’t hesitate to reach out to Lane and Associates Family Dentistry. Our team of dental professionals is here to help you achieve and maintain a smile you’re proud of!
Smile confidently and brightly—with just a bit of effort and care, a radiant smile is within your reach.